Children's bowel health - what's normal and what can go wrong.
Last Reviewed: October 2022
The bowels play an important role in maintaining your child’s general health from birth. Poo can tell us a lot about our body such as are we drinking enough and eating enough fibre.
Research shows many of us have no idea how to spot a common poo problem such as constipation. We find it uncomfortable to talk about and this can make it tricky to know if something is wrong and how to get help.
This page explains what a healthy bowel is and what normal poo should look like. There's also information on what can go wrong in our bowels and how you can help your child’s bowels work better.
Read our main factsheets Advice for children with constipation, Advice for children with daytime bladder problems and Advice for children with night time wetting for more information, including downloadable PDFs of the factsheets.
How bowels work
The bowel is a long tube-like organ which is part of our digestive system. This system begins when we put food into our mouths. Chewing food into little pieces makes it easier to swallow.
Our stomach then mashes the food into a soupy mixture before it gets passed into the small bowel. The body takes out the good stuff it needs (nutrients) before passing the rest of the waste liquid into the large bowel.
We have strong muscles in our large bowel that squeeze poo along (this movement is called peristalsis). As it travels through the bowel, water is removed turning poo into a smooth sausage shape.
When poo reaches our bottom, it stretches the muscles of our rectum. This sends a signal to our brain to tell us that a poo is waiting to be released. It can help to think of this as an internal warning system giving us time to find a toilet and empty our bowel.
Watch this video to learn more about the digestive system and how poo is made:
What is a healthy bowel?
A healthy bowel is a one that is regular. It is important to know what poo should look like and what a normal bowel pattern is, so that you can spot if your child has a problem such as constipation.
Use our Poo diary and Poo checker (based on the Bristol Stool Chart) to keep track of your child’s bowel habits. We even have a cake recipe for your child to bake to make checking poo types more fun!
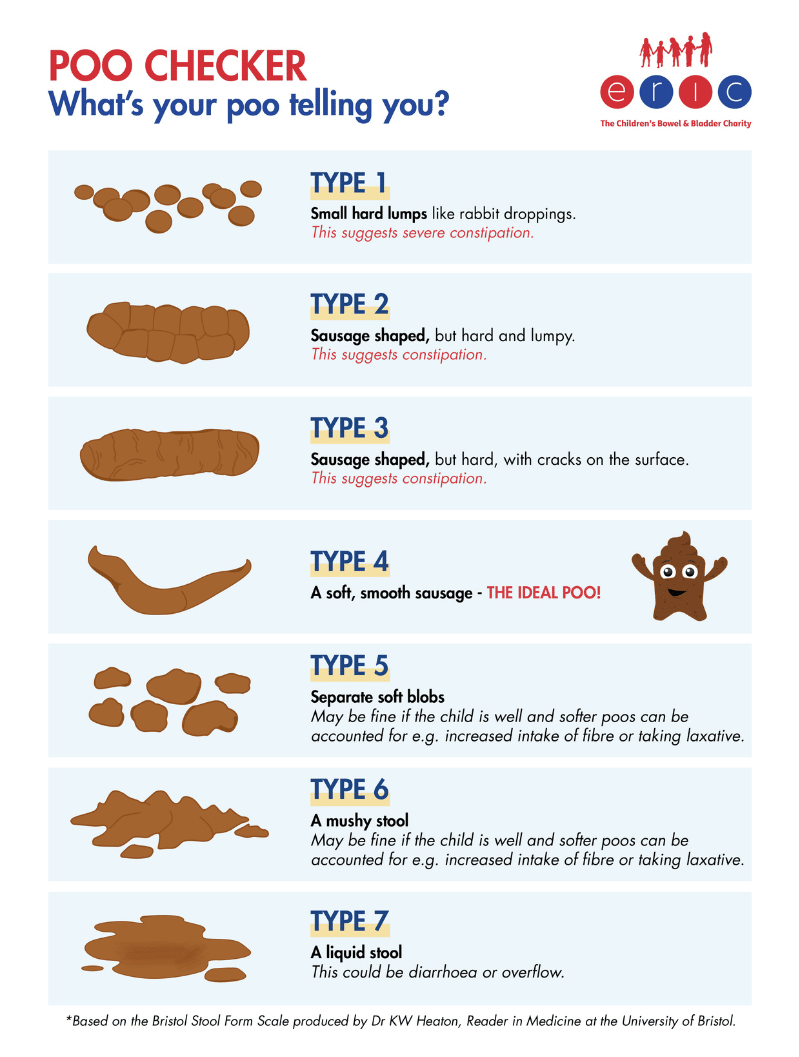
Look at our factsheet Advice for children with constipation for more information on what the other types of poo mean and how to get help for your child.
What is normal bowel function?
Normal bowel function is:
- When you first feel the urge to poo you can hold on long enough to get to a toilet without accident.
- Doing a poo within a minute of sitting on the toilet, it doesn’t hurt, and you don’t have to strain
- You completely empty your bowel, you don’t have to go back again, or have a feeling of some “left”.
- It is normal for you to feel an urge to poo within about half an hour of eating. This is known as the 'gastrocolic reflex' or peristalsis and is what prompts people to want to go to the toilet in the morning.
- A normal bowel pattern can range from several times a day to several times a week. It’s a good idea to pay attention to what your bowel habit is.
How often should children poo?
When the bowel is working normally, children should produce a soft, easy to pass poo at least 4 times a week. Ideally, children should pass some soft poo every day.
The time it takes our digestive system to turn food into poo is called our bowel transit time. The average time a child’s body takes to make poo is between 24 and 36 hours (which is a bit faster than an adult).
Why not try our sweetcorn test to see what your transit time is!
Baby’s bowels
Babies' bowel movements change as they go from new-born to the weaning stage (eating solid food) and beyond. The type and amount of poo they pass can also be affected by the sort of milk they are given (breast or formula).
Read more about bowel movements in children aged 0-5 years.
Tips for healthy bowels
- Drink plenty (at least 6-8 drinks a day) to keep poo soft.
- Eat lots of different foods including fruit and vegetables to help keep poo soft.
- Keep active. Running around and playing games helps to keep poo moving through your child's body.
- Have a regular routine of sitting on the toilet every day, especially after eating.
- Make sure your child sits with their feet flat on the floor and their knees raised above their hips, using a step if necessary
Common bowel problems in children
- Constipation affects 1 in 3 children. It is particularly common in children under 5 years old. The majority of these children have what is known as ‘functional constipation’. This means there is no underlying physical cause or other medical condition.
- Chronic constipation (faecal impaction)
- Soiling (encopresis)
- Withholding poo
- Children with additional needs such as autism are more likely to be affected by tummy problems and constipation.
- Toddler diarrhoea (Not to be confused with overflow soiling caused by constipation).
There are also conditions such as Hirschsprung’s disease and Spina Bifida which affect a small number of children from birth. Our Guide for Children with Complex Bladder and Bowel Problems is something you can read with your child.
Causes of bowel problems
- Passing a painful poo.
- Illnesses such as a stomach bug or fever which causes runny poo (diarrhoea).
- Some medications, such as painkillers can cause poo problems.
- Coeliac disease or a food intolerance
- A change in routine such as potty training, starting school and feeling anxious about doing a poo away from home can make it hard to relax and do a poo.
- A neurogenic bowel is caused by a nerve problem and causes a loss in bowel function/incontinence.
NHS England video about keeping bowels healthy
A short video recorded by ERIC nurse, Brenda Cheer with tips on keeping your child's bowel working properly and getting poo in the loo.
Resources
- All
- Kid's stuff
- Factsheets
- For Parents
- Fun Stuff
- Videos
Further help and information
If you are concerned about your child's bowel problems, book an appointment to see your G.P.
How to spot constipation symptoms in children, understand the causes and how to relieve the symptoms of constipation.
Learn how poo withholding can affect your child and what you can do to help them to feel more positive about going to the loo.
The colour, consistency and frequency of your baby’s poo can tell you a lot about their general health and development.
Children with autism or a learning disability are more likely to have tummy problems and become constipated. Find out why and get tips to help.
Download a free toilet pass from Bladder & Bowel Community to help your child access toilets discreetly.
Upcoming events
Share this page