Advice for children with night time wetting
Bedwetting in childhood is very common, affecting 1 in 15 seven year olds and 1 in 75 teenagers. It runs in families, but it’s no-one’s fault.
You don’t need to wait for your child to grow out of it – treatment is available from 5 years old (as per NICE Guidelines).
First of all, we have to work out WHY your child is wet – there are lots of different reasons all with their own special treatment.
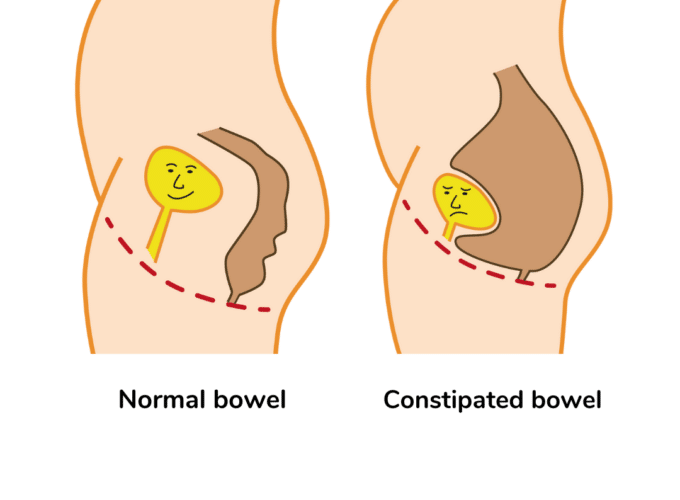
Constipation can cause night time wetting:
- The full bowel occupies the space in the tummy where the bladder wants to expand and fill.
- There isn’t enough space in the bladder to accommodate all the night time wee, so it leaks out.
- Constipation can go unnoticed except for the bedwetting, so ALWAYS check the bowel out first.
- ERIC’s Advice for Children with Constipation explains more about spotting the signs and what to do.
Some children have bladder problems in the daytime too:
- This might include frequency/urgency/daytime wetting.
- Urinary Tract Infections (UTIs) can also cause night time wetting.
- Daytime bladder problems need to be sorted before investigating night time issues. Read ERIC’S Advice for Children with Daytime Bladder Problems to find out how the bladder works and how to look after it, following the 4 steps to a healthy bladder.
Healthy bladder management and still wet?
It’s time for a bedtime checklist:
- Work on getting the drinking right in the daytime – plenty of it, evenly spread out, and thinking about what they drink – but also work on a good bedtime drinking routine. STOP drinks one hour before bedtime, every night, and no more after that until morning.
- Practise a good bedtime toileting routine. Schedule a relaxed toilet sit as part of preparing for bed, and pop back to the toilet just before sleep if it’s more than ½ an hour later.
- Have a trial without nappies. Even if nappies are always wet, try removing them for at least a week, preferably two, otherwise your child will never feel wet when they wee. It may be just the trigger they need to wake up.
- Protect the bed. Take the stress out of bedwetting by investing in a waterproof mattress cover, and waterproof duvet and pillow protectors if your child is really wet. Use an absorbent sheet to contain the wee too. Visit ERIC’s online shop for a wide range of bedding protection.
- Prepare your child for sleep. Unwind with a book or listen to music with the lights turned low. NO screens – so no TV, iPad, computer games in the hour before sleep, or the brain will get the wrong message.
- Help your child to practise taking themselves to the toilet if they wake. Think about a gentle night light or a torch so it’s not too dark. Should they go to the bathroom or use a potty/bucket/bottle in their bedroom? Are they in bunk beds? Make sure it is the bottom bunk. Practise pulling pyjamas up and down, and changing them if they get wet.
- Avoid lifting – in other words waking your child to take them to the toilet. It might keep the bed dry, but it encourages the child to wee during sleep as they don’t really wake up.
- Reward each step along the way – such as getting the drinking right, doing a bedtime wee and using the toilet at night.
If bedwetting persists after working on the 4 steps to a healthy bladder and practising a really good bedtime routine using the bedtime checklist, then it’s time to see the GP or nurse at a bedwetting clinic. Treatment is available from 5 years old.
What else causes bedwetting?
Some children find it hard to wake up when they need a wee.
It’s not because they are too fast asleep – it's because their brain just doesn’t recognise the signal of a full bladder during sleep. This is often called 'poor arousability'.
How will I know?
- Sleeping though wetting
- Wetting later in the night
- Moderate sized wet patches
- Normal concentration wee
Some children get really wet.
We all make vasopressin – a special hormone – at night. It tells our kidneys to make less wee while we sleep. Some children don’t yet make enough vasopressin so their kidneys produce lots of dilute wee – too much to fit inside their bladder.
How will I know?
- Wetting in the first 2 – 3 hours after going to sleep
- Large volume wetting
- Dilute wee
Some children's bladders don't stretch enough to hold all the wee they make at night.
How will I know?
- Wetting more than once at night
- May wake after wetting
- Small volume wetting
- Normal concentration wee
Some children are wet for more than one of these reasons.
Assessment
- Complete a Night Time Diary for at least a week. Looking at the detail of their wetting will help to work out the main reason why your child is wet.
- Take the diary to your appointment. The doctor or nurse will ask lots of other questions, finding out if your child has ever been dry at night, how their bladder behaves in the daytime, how often they poo etc.
- They will also ask how bothered your child is by their wetting. Working towards night time dryness is hard work; both child and parents need to be motivated in order to achieve success.
Specific treatments
Bedwetting alarm: a bedwetting alarm is likely to be the ideal treatment for 'poor arousability'. Bedwetting alarms have a sensor which detects when wetting starts. That activates an alarm which wakes the child (and/or parents) up.
Waking up makes the bladder muscles tighten so the child stops weeing. Over time, the alarm going off will help the child to associate the feeling of a full bladder with the need to get up and go to the toilet.
They will then learn to respond to the signal without needing to use the alarm; they will either wake to go to the toilet, or tell the bladder muscles to hold on and wait until morning.
Bedwetting alarms may be loaned from your local clinic or purchased from the ERIC online shop. A Bedwetting Alarm Diary can be used to monitor progress.
Desmopressin: a medication called Desmopressin can be taken to top up the child’s vasopressin. It is taken shortly before bedtime and tells the kidneys to produce less wee for 8 hours, so the bladder should be able to hold on until morning.
It can be more effective to take it an hour before bedtime so that it is already working on slowing wee production as the child prepares for bed.
There are strict instructions to follow like stopping drinking one hour before taking it, and not drinking for 8 hours after taking. There must be a week off the medication every 3 months to assess for ongoing need.
Overactivity: if the bladder is not stretching enough, and the child is passing frequent small wees, first double check for constipation. Then make sure the child is drinking correctly.
Persisting symptoms could be due to overactivity, when the bladder squeezes when it shouldn’t. The treatment for this is a medication such as Oxybutynin or Tolterodine.
Combination treatment: combination treatment may be required for children who are wet for more than one reason. The best possible treatment should be chosen. Then if wetting persists, the treatment should be continued and the Night Time Diary repeated. Then another treatment can be added.
More info
- Video: Become a Bedwetting detective
- Bedwetting Alarms - your questions answered
- Flowchart - Night Time Wetting (part of our Children's Continence Pathway)
- Helpline podcasts
- Desmopressin Factsheet
Last Reviewed: January 2024
Next Review: January 2027
Upcoming events
Share this page