Physical examination for constipation
Why every child needs a full physical examination when diagnosed with constipation
ERIC nurse, Brenda Cheer, explains why an abdominal examination alone isn't enough to diagnose a poo problem and how important a full physical examination is.
Read on to find out how doctors should assess all children, what they should be looking for and what to do if you're worried your child hasn't been properly checked over.
The doctor has felt her tummy and says she is not constipated...
How often do we hear that said by frustrated callers to our Helpline...but how is it even possible for a doctor to reach that conclusion after a quick abdominal examination? They may be able to feel lumps of hard stool – but if they don’t feel any, that doesn’t rule out constipation.
If the child is slim, abdominal palpation may be fairly reliable, but a chubby tummy makes it much more difficult. And children can be full of soft poo – not much to feel then.
How should constipation be diagnosed?
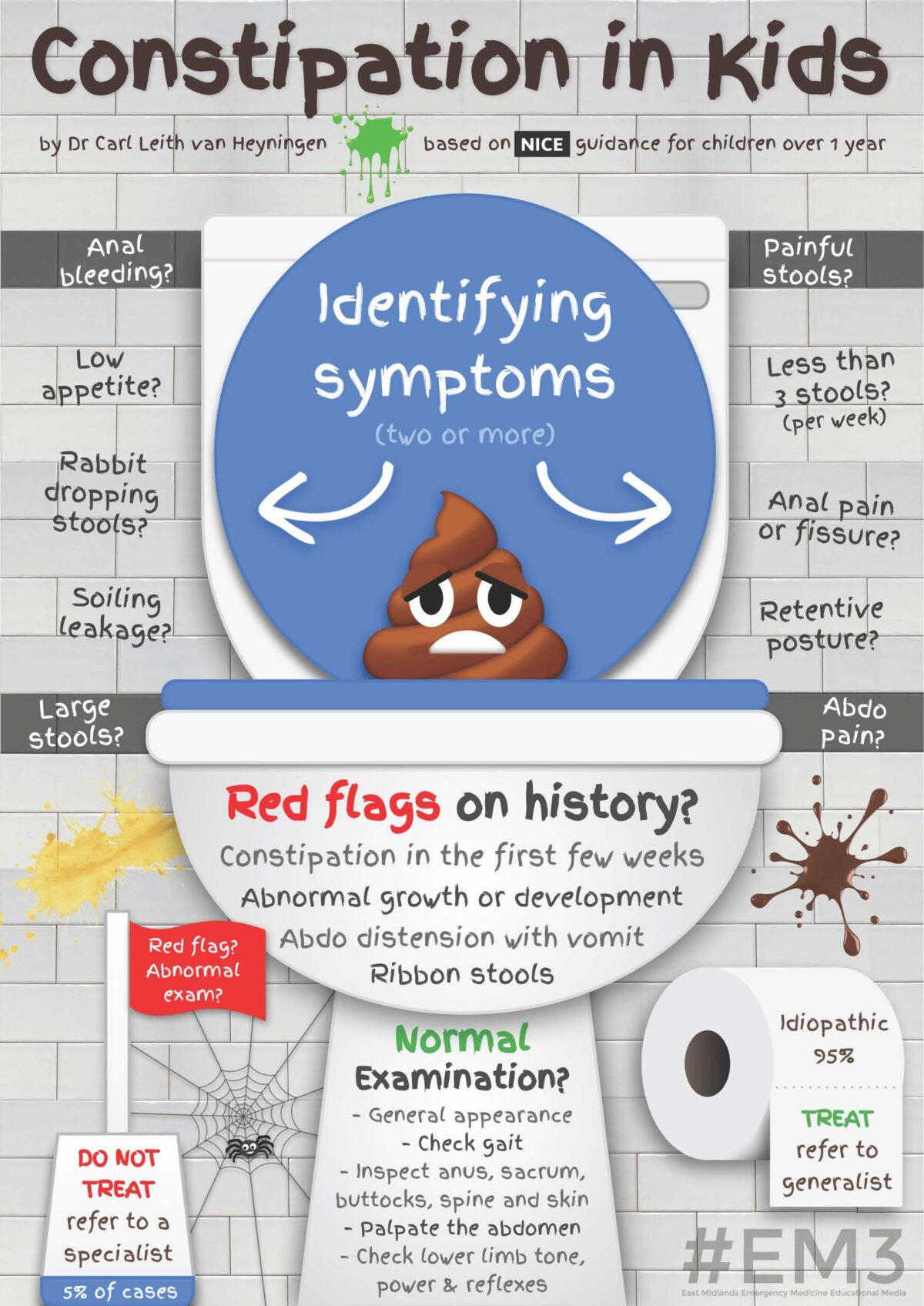
Constipation is diagnosed by taking a detailed history – of the consistency of stools, frequency of bowel actions, appetite, behaviour, soiling…all included in the Continence Assessment Form – part of ERIC’s generic Children’s Continence Pathway. This tool was developed from the NICE Guidelines and is a model of best practice for assessing and treating children’s bowel and bladder problems.
Why a full examination is so important
There’s a danger that focussing on feeling the tummy distracts from the importance of the full examination. Any child presenting with constipation must have a physical examination to rule out any underlying organic cause.
In other words, we have to make sure the child doesn’t have a bowel condition, or a neurological problem stopping the signal of a full bowel reaching the brain.
The Constipation Flowchart on our Children’s Continence Pathway makes it clear what needs to be done:
- Check appearance of anus and surrounding area to exclude anorectal anomaly
- Check lower limb neurology and appearance of spine to exclude neurological link e.g. spinal anomaly
- Check for abdominal mass
- Check for faltering growth (slower rate of weight gain than expected for their age and gender)
Why is this so important? The vast majority of constipation is functional – in other words there is no underlying condition. But sometimes it isn’t…
How underlying problems can be missed
Sara was nearly five years old when she was diagnosed with Spina Bifida. Almost five years of parental anxiety, battling with intractable, hard to control constipation. A good two years of suffering for a very bright little girl, who worked so hard at potty training, but just couldn’t stop the wee and poo leaking out. Years of battling with GP, Health Visitor, paediatrician – it was obvious to her parents that something was wrong but no-one believed them.
True, Sara is not a typical presentation – there is nothing to see on her spine and she’s a very active little girl. But all someone needed to do was check her lower limb neurology – in other words look for the knee and ankle jerks, the reflexes that should have been there, but weren’t.
This poster created by Dr Carl Leith van Heyningen is a great visual guide to 'red flags':
Sara is just one example, but unfortunately she is by no means the only child to be let down by the doctors and nurses who should have looked after her. No doctor can know everything about every possible condition, but every doctor can follow well publicised guidance instead of relying on ‘magic fingers.’
What can parents/carers who think their child has a poo problem do?
If you think your child could be constipated, take a look at our signs of constipation and our Advice for Children with Constipation factsheet before booking an appointment with your GP.
Use ERIC's poo diary to keep track of their bowel habits for a few days - note down what it looks like using the Bristol Stool Chart, how often they're going and if they're in any pain.
Book an appointment for your child to be assessed by your GP. Ask the receptionist if there's a doctor available with experience of treating childhood constipation.
Make sure the doctor does a full examination following The Constipation Flowchart on our Children’s Continence Pathway.
If you've been to the doctor and they only felt your child's tummy, then go back! Ask to see a different doctor and print out this page to take with you.
Upcoming dates
Share this page